
In patients with SR at baseline, arrhythmia was induced by programmed, incremental, or burst atrial pacing. The key exclusion criteria were complex congenital heart defects (corrected or uncorrected), isolated post-capillary PH, previous RFCA for AF, AT or AFL, NYHA Class IV, and life expectancy 300 s during the procedure. 17 Patients were excluded if they had any condition that might jeopardize patient safety or limit their participation in the study. Participants were men or women, 18 years of age or older, who had pre-capillary or combined post- and pre-capillary PH of any aetiology, and documented symptomatic AF (paroxysmal, persistent, or long-standing persistent) or AT (typical AFL included) who were indicated for RFCA according to clinical practice guidelines.
#Atrial flutter ablation cpt trial#
The trial protocol is available in Supplementary material online, Appendix S1. Individual written consent was obtained from each patient. The multicentric and local Ethics committees at all centres approved the study protocol. It was performed according to good clinical practice and in compliance with the Helsinki declaration. The study was a multicentre, parallel-group, open-label, randomized trial. We investigated this hypothesis in a randomized fashion. not only ablation for index arrhythmia) could reduce the risk of arrhythmia recurrence and improve the clinical outcomes compared to procedure targeting the clinical arrhythmia only. Given the knowledge of the sequential manifestation of different SVTs in individual patients, it was plausible to hypothesize that first-line bi-atrial RFCA of all potentially arrhythmogenic substrates (i.e. 3–6 In this respect, data on the optimum rhythm control strategy of AF/AT, including RFCA, is lacking.

13, 14Īlthough typical AFL can frequently be found as the first manifestation of SVT in patients with PH, atrial fibrillation (AF) is even more prevalent. 13, 14, 16 Importantly, new-onset arrhythmias (different than their index SVT) were observed in 30–48% of recurrent cases. 5, 10, 13–16 However, the long-term results were much less favourable with freedom from arrhythmia in only 50–78% of patients. Radiofrequency catheter ablation (RFCA) of typical atrial flutter (AFL), atrioventricular nodal re-entrant tachycardia (AVNRT), and other focal or macroreentrant atrial tachycardias (AT) was reported to be effective (acute success rate of 86–100%) and safe in patients with PH according to retrospective studies with a limited number of patients. 3, 6, 10 However, antiarrhythmic drugs may not be a feasible option because of their negative inotropic properties and interaction with specific therapy for PH. 3, 4, 6, 9 Conversely, maintenance of sinus rhythm (SR) appeared to improve the clinical outcome. 8 The SVTs are associated with clinical deterioration and adversely impact the prognosis. Supraventricular tachycardias (SVTs) have been frequently observed with a cumulative incidence of 10–29% in patients with both idiopathic 3 and secondary PH, 4–7 including chronic thromboembolic pulmonary hypertension, either inoperable 4, 6 or treated with pulmonary endarterectomy.
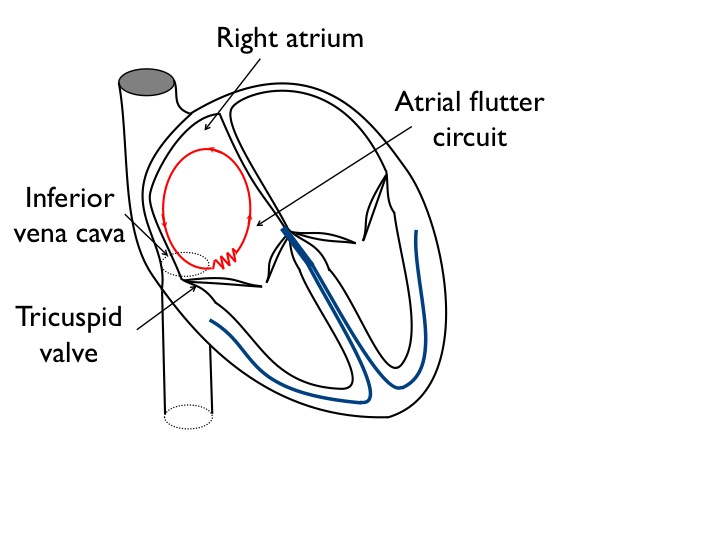
1, 2 Despite those advancements, PH is still a progressive disease with a generally inauspicious prognosis. Various treatment strategies have been established in patients with pulmonary arterial hypertension (PH) that improve haemodynamics, exercise capacity, and quality of life. There was no excess of procedural complications and clinical follow-up events including an all-cause death in the Extended ablation group.Įxtensive catheter ablation does not reduce arrhythmia recurrence in patients with pulmonary hypertension and atrial fibrillation/tachycardia.ĭespite enormous right atrial enlargement, regions with low-voltage and/or abnormal atrial electrograms are rare in patients with pulmonary hypertension. Limited ablation group (hazard ratio: 0.97, 95% confidence interval: 0.49–2.0). During the median follow-up period of 13 (interquartile range: 12 19) months, the primary endpoint occurred in 15 patients (42%) vs. The presumable clinical arrhythmia was AF in 38 and AT in 36 patients, including typical AFL in 23 patients. A total of 77 patients (mean age 67 ± 10 years 41 males) were enrolled. The primary endpoint was arrhythmia recurrence >30 s without antiarrhythmic drugs after the 3-month blanking period.
#Atrial flutter ablation cpt plus#
Patients underwent either clinical arrhythmia ablation only (Limited ablation group) or clinical arrhythmia plus substrate-based ablation (Extended ablation group). Patients with combined post- and pre-capillary or isolated pre-capillary PH and supraventricular arrhythmia indicated to catheter ablation were enrolled in three centres and randomized 1:1 into two parallel treatment arms.


 0 kommentar(er)
0 kommentar(er)
